Silcare Breathe™ Walk (perforated liner)
The importance of the right liner
Optimal control of a prosthetic limb depends on a comfortable and secure connection between the residual limb and the socket. Modern liner technology provides excellent cushioning, but the impermeable and insulating materials can allow a build-up of heat and moisture so they begin to slip and chafe. Air, perspiration and unnecessary movement can cause a loss of connection, compromised stability and damage to residual skin, potentially affecting mobility, safety and independence.
Silcare Breathe™
The patented technology of Silcare Breathe™ works by letting air and perspiration that are often trapped between the liner and skin, to escape through specially designed laser drilled perforations. The air and moisture are then expelled from the socket as the wearer walks, resulting in drier skin and a healthier environment for the residual limb. This helps to increase comfort and control, and reduce the damaging effects of relative motion on damp tissues that is often encountered with standard prosthetic liners.
Silcare Breathe™ Walk uses a softer silicone, making it suitable for more active users i.e. those who have an activity level of 2.
- Activity level 2
Key Benefits
-
Improved Limb Health

Perforated liners reduce the need to remove prosthesis throughout the day to dry residual limb, compared to non-perforated liners, delivering improvements in residual limb health and wound healing.
-
Sweat Management

Optimally sized pores distributed uniformly along the length and distal end of the liner permit the escape of moisture, removing sweat from skin-liner interface.
-
More Reliable Fit

Firmer silicone allows a firmer connection between the residual limb and the liner.
-
Improved Comfort
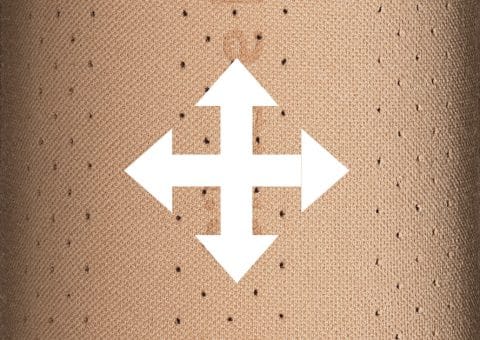
Seamless knitting technology provides bi-directional stretch to improve comfort and contouring, and reduce shear force on the knee as it flexes. Use with a one-way valve on the socket helps to generate a better vacuum and more secure fit.
-
Reduced stress on skin

Tendresse™ finish provides a lower coefficient of friction than standard silicone, reducing shear stresses on the skin.
-
Temperature Regulation
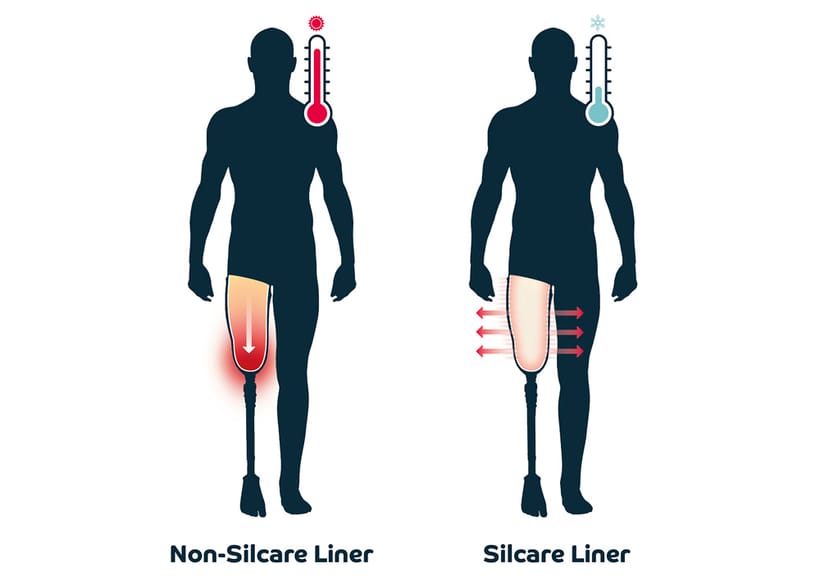
Improved heat dissipation compared to other temperature regulation solutions.
Available in both Cushion and Locking system
Cushion System
- Use in conjunction with a one way valve and airtight suspension sleeve helps to generate a better vacuum and more secure fit.
Locking System
- Uni-directional stretch distally resists pistoning whilst bi-directional stretch proximally
allows for comfortable knee flexion. - Locking system and unique one way valve create an airtight seal between the skin and
the inner surface of the liner. No separate suspension sleeve is required making knee
flexion easier, creating a cooler environment for skin and a more comfortable limb and
socket connection.
Silcare Breathe™ Technology
The body cools by moving blood flow closer to the surface of the skin, and when this is not sufficient the body produces sweat to increase cooling by evaporation.
The need to regulate body temperature is greater for amputees, and a lack of temperature regulation can have severe negative effects.

The Silcare Breathe™ range has been designed to tackle these issues. Laser drilled perforations transmit moisture away from the skin to ensure a comfortable, cool and secure fit for the user.
- Reduced relative movement between the residual limb and liner
- Enhanced proprioception
- Enhanced comfort
- Drier, cooler, healthier skin
1 Seymour,R. Prosthetics and Orthotics: Lower Limb and Spinal. Philadelphia: Lippincott, Williams and Wilkins 2002,
2 Hagberg K, Brånemark R. Consequences of non-vascular trans-femoral amputation: a survey of quality of life, prosthetic use and problems. Prosthetics and Orthotics International. 2001; 25(3):186-94.
3 Peery JT, Ledoux WR, Klute GK. Residual-limb skin temperature in transtibial sockets. Journal of Rehabilitation Research & Development. 2005; 42(2):147-54.
Testimonials
Silcare Breathe™ Liner Clinical Evidence Reference
Clinical Outcomes using Sweat Management liners
-
Residual Limb Health
- Improvements in residual limb health problems and wound healing1,2
- Fewer residual skin issues2
- Reduction in pain in residual and phantom limb2
- Improved heat dissipation compared to other temperature regulation solutions3
- Removes sweat from skin interface1,2,4
- Perforations do not damage the skin4
-
User satisfaction
- Patients reported a preference for their perforated liners1,4
- Reduces the need to remove prosthesis throughout the day to dry residual limb4
-
Clinical Outcomes using Silicone liners
There are two published literature reviews that discuss different aspects of lower limb prosthetic liner technology5,6.
- The main purpose of prosthetic liners is to cushion the transfer of loads from the prosthetic socket to the residual limb5.
- Based on load-displacement data from the compressive stiffness tests, silicone was one of three materials that were recommended for situations where it is desirable for the liner to maintain thickness and volume since these materials had the least non-recovered strain5,7.
- Under cyclic compressive loading, silicone was one of two materials that had the greatest cycles to failure under compressive loading, while the Pedilin and polyurethane samples lasted orders of magnitude less5,8.
- Prosthetic liners and sockets are highly resistive to heat conduction and could be a major contributor to elevated skin temperatures5,9.
- There are reduced residual limb pressures with the silicone liner compared to other conditions (no liner; soft inserts) suggesting that silicone has an ability to distribute pressure evenly to the residual limb4,10.
- In terms of patient outcomes, there was no clear preference between silicone and Pelite liners5,11.
References
-
Full Reference Listing
-
McGrath M, McCarthy J, Gallego A, et al.
The influence of perforated prosthetic liners on residual limb wound healing: a case report. Can Prosthet Orthot J 2019; 2(1).
-
Davies KC, McGrath M, Stenson A, Savage Z, Moser D, Zahedi S.
Using perforated liners to combat the detrimental effects of excessive sweating in lower limb prosthesis users. Can Prosthet Orthot J. 2020;3(2).
-
Williams RJ, Washington ED, Miodownik M, et al.
The effect of liner design and materials selection on prosthesis interface heat dissipation. Prosthet Orthot Int 2018; 42: 275–279.
-
Caldwell R, Fatone S.
Technique for perforating a prosthetic liner to expel sweat. JPO J Prosthet Orthot 2017; 29: 145–147.
-
Klute GK, Glaister BC, Berge JS.
Prosthetic liners for lower limb amputees: a review of the literature. Prosthet Orthot Int 2010; 34: 146–153.
-
Richardson A, Dillon MP.
User experience of transtibial prosthetic liners: a systematic review. Prosthet Orthot Int 2017; 41: 6–18.
-
Sanders JE, Greve JM, Mitchell SB, et al.
Material properties of commonly-used interface materials and their static coefficients of friction with skin and socks. J Rehabil Res Dev 1998; 35: 161–176.
-
Emrich R, Slater K.
Comparative analysis of below-knee prosthetic socket liner materials. J Med Eng Technol 1998; 22: 94–98.
-
Klute GK, Rowe GI, Mamishev AV, et al.
The thermal conductivity of prosthetic sockets and liners. Prosthet Orthot Int 2007; 31: 292–299.
-
Sonck WA, Cockrell JL, Koepke GH.
Effect of liner materials on interface pressures in below-knee prostheses. Arch Phys Med Rehabil 1970; 51: 666.
-
Lee WC, Zhang M, Mak AF.
Regional differences in pain threshold and tolerance of the transtibial residual limb: including the effects of age and interface material. Arch Phys Med Rehabil 2005; 86: 641–649.
-